CITIZEN TRIBUNE
Health
EEE-2
Tuesday, October 24, 2017
Millions die suffering amid global opioid gap, report says
WASHINGTON (AP) — Near-
ly 26 million people around the
world die each year with serious
suffering in part because of a huge
gap in pain relief: The U.S. may
be awash in opioid painkillers, but
they're rare or unavailable in doz-
ens of poor countries, says a new
report.
The challenge is to improve pal-
liative care in low-income coun-
tries while avoiding mistakes that
led to the U.S. addiction crisis.
The report to be published Fri-
day in The Lancet says one key
is using off-patent morphine that
costs pennies a dose — not profit-
able for drug companies that push
pricier, more powerful opioids in
rich countries, but critical to eas-
ing a health emergency.
In some places, even children
dying of cancer or children in
treatment for cancer can't get pain
relief, said University of Miami
professor Felicia Knaul. She co-
chaired a Lancet-appointed inter-
national commission that spent
three years studying the disparity
and what she calls "the moral ob-
ligation" to help.
"This report finally gives voice
to the suffering and a roadmap to
governments," Knaul said.
Of the few hundred tons of
morphine and equivalent opioids
distributed worldwide, less than 4
percent goes to low- and middle-
income countries, the researchers
reported.
How much is needed? The Lan-
cet Commission provided the first
global estimates of the need for
palliative care, defined as "seri-
ous health-related suffering" from
certain life-threatening condi-
tions, including cancer, HIV and
trauma.
Some 2.5 million children are
among the annual count of nearly
26 million who die without ad-
equate relief, the team calculated.
Another 35.5 million people a
year have serious pain and suf-
fering from those conditions but
aren't dying, and most live in low-
or middle- income countries.
The world's poorest countries
have access to enough morphine
to meet less than 2 percent of their
palliative care needs, the report
found. India fares little better, at
4 percent; China meets 16 percent
of its need, and Mexico 36 per-
cent.
The 2010 earthquake in Haiti
highlighted the scarcity, as doc-
tors lacked opioids for people who
were severely injured or needed
surgery, the commission noted.
Beyond painkillers, the panel
urged health systems to make
available an "essential pack-
age" of palliative care services
that also includes medications to
ease breathing problems, muscle
spasms, complications of heart or
liver failure, and depression and
psychological suffering. The list
also includes practical equipment
like pressure sore-reducing mat-
tresses, adult diapers — and a lock
box for any needed morphine.
The Lancet panel looked to les-
sons from the U.S. opioid crisis,
and from Western Europe, which
has avoided similar abuse thanks
to strict opioid monitoring and
to universal health coverage for
non-opioid treatments for chronic
pain, said report co-author Dr.
Lukas Radbruch, a palliative care
specialist at Germany's University
of Bonn.
Among the recommendations:
-Countries should use cheap,
immediate-release oral and inject-
able morphine for severe pain.
Closing the pain gap would cost
$145 million.
—Don't allow drug company
marketing to patients, physicians
or other health care providers. In
the U.S., prescriptions soared af-
ter marketing of newer opioids for
less severe types of pain.
—Closely monitor morphine
supply, and train health workers
in proper pain treatment.
The $1.5 million study was
funded by the University of Mi-
ami and Harvard University and
with grants including from the
U.S. National Cancer Institute,
American Cancer Society and
drug maker Pfizer. Another drug
company, Roche, provided a grant
to help the University of Miami
disseminate the findings.
One specialist who has long
warned that the U.S. addiction
crisis could spread internationally
said the proposal for poor coun-
tries to avoid patented opioids was
a "sensible" approach.
Still, "I wish they had included
a stronger warning regarding the
risks of a pain management agen-
da being co-opted by profit-seek-
ing pharmaceutical companies as
it was in the United States," said
Stanford University psychiatry
professor Keith Humphreys, who
wasn't involved in the Lancet re-
port.
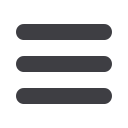
SAN DIEGO (AP) —
Doctors were just guessing a
decade ago when they gave
Alison Cairnes' husband a
new drug they hoped would
shrink his lung tumors. Now
she takes it, but the choice
was no guesswork. Sophisti-
cated gene tests suggested it
would fight her gastric can-
cer, and they were right.
Cancer patients increas-
ingly are having their care
guided by gene tumor
boards, a new version of
the hospital panels that tra-
ditionally decided whether
surgery, radiation or chemo-
therapy would be best. These
experts study the patient's
cancer genes and match
treatments to mutations that
seem to drive the disease.
"We dissect the patient's
tumor with what I call the
molecular microscope," said
Dr. Razelle Kurzrock, who
started a board at the Univer-
sity of California, San Diego,
where Cairnes is treated.
It's the kind of care many
experts say we should aim
for — precision medicine,
the right drug for the right
person at the right time,
guided by genes. There are
success stories, but also
some failures and many
questions:
Will gene-guided care im-
prove survival? Does it save
money or cost more? What
kind of gene testing is best,
and who should get it?
"I think every patient
needs it," especially if can-
cer is advanced, said Kurz-
rock, who consults for some
gene-medicine companies.
"Most people don't agree
with me — yet. In five years,
it may be malpractice not to
do genomics."
Few people get precision
medicine today, said Dr. Eric
Topol, head of the Scripps
Translational Science Insti-
tute. "The only thing that's
gone mainstream are the
words."
HOW IT WORKS NOW
If you have a cancer that
might be susceptible to a
gene-targeting drug, you
may be tested for mutations
in that gene, such as HER2
for breast cancer. Some
breast or prostate cancer pa-
tients also might get a multi-
gene test to gauge how ag-
gressive treatment should be.
Then most patients get
usual guideline-based treat-
ments. If there's no clear
choice, or if the disease has
spread or comes back, doc-
tors may suggest tumor
profiling — comprehensive
tests to see what mutations
dominate.
That's traditionally been
done from a tissue sample,
but newer tests that detect
tumor DNA in blood — liq-
uid biopsies — are making
profiling more common. The
tests cost about $6,000 and
many insurers consider them
experimental and won't pay.
Gene tumor boards ana-
lyze what the results suggest
about treatment. They focus
on oddball cases like a breast
cancer mutation in a colon
cancer patient, or cancers
that have widely spread and
are genetically complex. The
only options may be experi-
mental drugs or "off-label"
treatments — medicines
approved for different situa-
tions.
But as tumor profiling
grows, it's revealing how
genetically diverse many
tumors are, and that oddball
cases are not so rare, said
Dr. John Marshall. He heads
the virtual tumor board
at Georgetown Lombardi
Comprehensive
Cancer
Center that also serves can-
cer centers in Pennsylvania,
North Carolina, Michigan
and Tennessee.
"There is a little bit of
faith" that testing will show
the right treatment, but it's
not a sure thing, said Dr. Lee
Schwartzberg, who heads
one participating center,
the West Cancer Center in
Memphis.
Dr. Len Lichtenfeld, the
American Cancer Society's
deputy chief medical officer,
is optimistic yet wary. Drugs
that target BRAF mutations
work well for skin cancers
called melanomas, but less
well for lung or colon can-
cers.
"Just because a mutation
occurs it doesn't mean that
drug is going to work in that
cancer," he said.
LUCKY CASES
When it does, results can
be dramatic. Cairnes' can-
cer was between her stom-
ach and esophagus, and had
spread to her liver, lungs and
lymph nodes. Tissue testing
found 10 abnormal genes,
but on the liquid biopsy only
EGFR popped out as a good
target.
Two drugs aim at that
gene but aren't approved for
her type of cancer. A tumor
board advised trying both
— Erbitux and Tarceva, the
drug her husband also had
taken.Within two weeks, she
quit using pain medicines.
After two months, her liver
tumor had shrunk roughly
by half. There are signs that
cancer may remain, but it is
under control. She feels well
enough to travel and to take
care of her granddaughter.
"I'm very, very grateful
to have a targeted therapy,"
Cairnes said.
"I cannot expect a better
outcome than what we're
seeing right now," said her
doctor, Shumei Kato.
WHAT STUDIES SHOW
But is gene-guided treat-
ment better than usual care?
French doctors did the first
big test, with disappointing
results. About 200 patients
with advanced cancer were
given whatever their doc-
tors thought best or off-label
drugs based on tumor profil-
ing. Survival was similar —
about two months.
Another French study, re-
ported in June, was slightly
more encouraging on sur-
vival but exposed another
problem: No drugs exist
for many gene flaws. Tests
found treatable mutations in
half of the 2,000 participants
and only 143 got what a tu-
mor board suggested.
Some doctors worry that
tumor boards' recommend-
ing off-label treatments di-
verts patients from research
that would benefit all can-
cer patients. For example,
the American Society of
Clinical Oncology's TAPUR
study tests off-label drugs
and shares results with their
makers and federal regula-
tors.
LETTING PATIENTS
CHOOSE
Ann Meffert, who lives on
a dairy farm in Waunakee,
Wisconsin, endured mul-
tiple standard treatments that
didn't defeat her bile duct
cancer.
"She was going to be re-
ferred to hospice; there was
not much we could do,"
said Dr. Nataliya Uboha,
who took the case to a tu-
mor board at the University
of Wisconsin-Madison. The
panel gave several options,
including off-label treat-
ment, and Meffert chose a
study that matches patients
to gene-targeting therapies
and started on an experimen-
tal one last October.
"Two weeks in, I started
feeling better," she said, and
when she saw test results, "I
couldn't believe the differ-
ence."
Many lung spots disap-
peared and the liver tumor
shrank 75 percent. She is
not cured, though, and doc-
tors are thinking about next
steps. And that could involve
a fresh look at her tumor
genes.
Gene tumor boards
guide cancer care
Ultra-personal Therapy
AP
Cancer patient Alison Cairnes poses for a portrait at the University of California San Diego
in San Diego, Calif., on Aug. 15, 2017. Doctors were just guessing a decade ago when they
gave Cairnes’ husband a new drug they hoped would shrink his lung tumors. Now she takes
it too, but the choice was no guesswork.
AP
In this Aug. 17, 2017 photo, doctors, pharmacists, geneticists and oth-
ers meet to discuss how to best treat cancer patients at the University
of Wisconsin Carbone Cancer Center in Madison, Wis.


















